The interim last guideline that would ban surprise billing is being dealt with by the media like among the best developments American health care has actually ever seen. To be sure, balance billing is so patently unreasonable that there is unusual bipartisan support for the proposed law, which may indeed safeguard consumers from this insidious practice. But its not the genuine answer to repairing a health care system that exploits its consumers.
Surprise medical billing is simply one symptom of an underlying problem– a system of incentives that rewards maximization of revenue from each patient encounter, combined with an incredible absence of accountability. That is how we end up with a healthcare system that damages one quarter of Medicare inpatients through omissions or mistakes, and how, even during a pandemic, we get health center systems suing countless former clients over expenses they cant pay– often bills they never ever expected because they were never ever informed what their costs would remain in advance. Its also why two-thirds of people submitting for insolvency state medical costs are an essential factor to their monetary problems.
After more than a decade of unobstructed combination, a lot of health centers are units of multibillion-dollar big services, using over half the physicians in the country– no longer the community resource they as soon as were. Significantly corporatized, healthcare facilities purchase doctor practices as possessions, and pressure those clinicians to create an ideal return on investment. Earnings maximization– not results that matter to patients or sensible use of resources– is the name of the game. Numerous doctors squander their practices to become part of this brand-new healthcare, and sometimes they are required to leave their ethical sensibilities behind.
The factor that some clinicians can justify the numerous trespasses of a corporatized healthcare delivery system is that it pays well and eliminates them of the burdens of running their own practices. One other reason is that neither they nor their business employers need to care much about whether they actually provide the results they promise to patients. They need to balance corporate pressure to “be a member of the team” versus what they understand is sensible clinical practice. The current system makes that tough, due to the fact that it pays them for every procedure, service, test, or consult they provide in taking care of patients– the more they do, the more they make. And if their business managers believe its fine to take advantage with surprise bills, well, so be it. Its no longer their issue. None of it will ever capture up with them.
And thats why we have surprise billing and all the other ills of our current healthcare system– due to the fact that there is no accountability for managing cost, quality, or even for pleasing clients. Up until Medicare and commercial insurers link the compensation they pay providers to the things that matter to us as consumers and people, we will continue to have an inefficient system that abides appalling practices like surprise billing, and continue to hang out on band-aids like this interim last guideline rather of fixing the real issue.
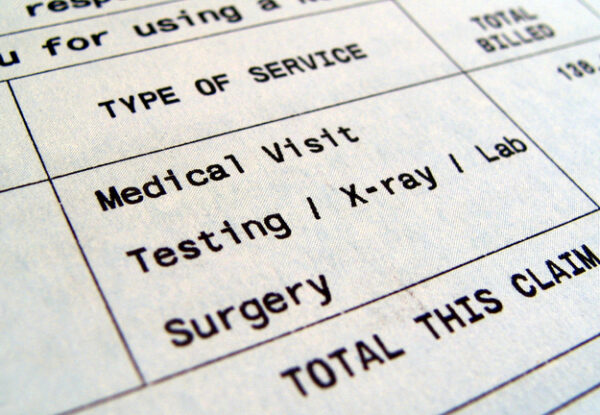
Image: lbodvar, Getty Images
Its not the genuine answer to repairing a healthcare system that exploits its consumers.
That is how we wind up with a healthcare system that damages one quarter of Medicare inpatients through omissions or errors, and how, even throughout a pandemic, we get healthcare facility systems suing thousands of former patients over bills they cant pay– typically expenses they never ever expected because they were never told what their expenses would be in advance. The factor that some clinicians can justify the numerous trespasses of a corporatized healthcare delivery system is that it pays well and eases them of the problems of running their own practices.